A reader wrote that her physician freaked out when she was told that the reader was consuming 15,000 IU of Vitamin D3. The physician was sure that she would have vitamin toxicity within a month!!
One of the problems is that labs use “local population” to define normal ranges for almost all lab results. For Vitamin D, this means that if you live in a vitamin D deficient area, you may be deficient and in the normal range!
Historically the old recommended dietary allowance was 200 IU/Day. In 2011, it was raised to 600 IU/day.
This was the level to prevent rickets. It was not the level to produce optimal health or minimize the risk of cancer or diabetes.
- “Several diseases have been linked to vitamin D deficiency, such as hypertension, diabetes, depression, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and chronic pain syndromes such as fibromyalgia. ” [2013]
- “Vitamin D deficiency was defined as a serum 25-hydroxyvitamin D concentrations ≤20 ng/mL (50 nmol/L). The overall prevalence rate of vitamin D deficiency was 41.6%,” [2011]
- “Older adults are advised to maintain serum 25(OH)D concentrations >75 nmol/L.” [2006]
- Dr. Mercola recommends 45-50 ng/ml or 115-128 nmol/l [source]
- “Vitamin D intakes required to maintain serum 25(OH)D concentrations of >80 nmol/L in 97.5% of the sample[of men and women aged 20-40 y] were … 41.1μg/d (1640 IU), respectively.” [2008]
- “The clinical trial evidence shows that a prolonged intake of 250 mug (10,000 IU)/d of vitamin D(3) is likely to pose no risk of adverse effects in almost all individuals in the general population; this meets the criteria for a tolerable upper intake level.” [2007]
- “Evidence from clinical trials shows, with a wide margin of confidence, that a prolonged intake of 10,000 IU/d of vitamin D(3) poses no risk of adverse effects for adults,” [2009]
- NOTE: there was no evidence going 50% higher has any risks. The studies just tested the 10,000IU level.
- “Vitamin D, important for maintaining bone health in Crohn Disease[CD], may have potential as a treatment for the core inflammatory disease process. There is plausible evidence in favour of vitamin D as an anti-inflammatory from animal models, epidemiological and cross sectional studies of CD.”[2015]
- “Active Crohn’s disease was associated with low serum 25-OH vitamin D.”[2013]
- “In addition, low vitamin D has been associated with disease activity in CD patients, and supplementation appears to be beneficial in improving clinical scores and reducing inflammation.” [2014]
- “Vitamin D is an inexpensive supplement which has been shown to improve IBD outcomes.”[2014]
- “people with IBD may remain in remission longer when treated with oral vitamin D…suggest that vitamin D may modify the immune response in IBD.” [2015]
Vitamin Council writes:
- “vitamin D toxicity is more likely to develop if you take 40,000 IU/day everyday for 3 months or more.
- take more than 300,000 IU in a 24 hour period.”
There is a formula that was developed for dosages to be received over several weeks
(IU)=40x(TargetLevel-serum 25-OHD(3))xbody weight (kg).
So, if my target is 128 nmol/l [Dr. Mercola] and I weight 120 kg and my current level is 20 nmol/l then:
(IU) = 40 (128 -20) x 120 = 40 * 108 x 120 = 648,000 IUs.
At 10000 IU/day, it would take 2 months to get that much in, provided there are no problem with absorption of Vitamin D (the above was done on healthy individuals).
“Absorption occurs primarily in the proximal small intestine and is influenced by gastric, pancreatic and biliary secretions, micelle formation, diffusion through the unstirred-water layer, brush-border-membrane uptake, and transport out of the intestinal cell (24). Any process resulting in malabsorption of intestinal fat may impair the absorption of vitamin D. In one study, absorption of tritium-labeled (3H)-vitamin D in normal subjects ranged from 62.4% to 91.3% of the initial oral dose (10). In patients with celiac disease, biliary obstruction absorption and chronic pancreatitis, absorption fell to 50%, < 28% and < 18% of the oral dose, respectively.” [2011]
“The researchers found that Crohn’s Disease patients had on average a 30 percent decrease in their ability to absorb vitamin D2 when compared to normal subjects.” [2011]
Working on the premise that CFS and FM are microbiome dysfunctions, they will likely also suffer from diminished absorption of Vitamin D. A paper by Anna Dorothea Höck, MD cites “Chronic fatigue syndrome, a condition of vitamin D resistance?”
Bottom Line
Studies have established that 10,000 IU/day is safe for well absorbing people with a wide confidence interval. With Crohn’s and other disease with microbiome disturbance, a 30% loss of absorption is seen, then 14285 IU/day is needed to net the 10,000 IU’s above.
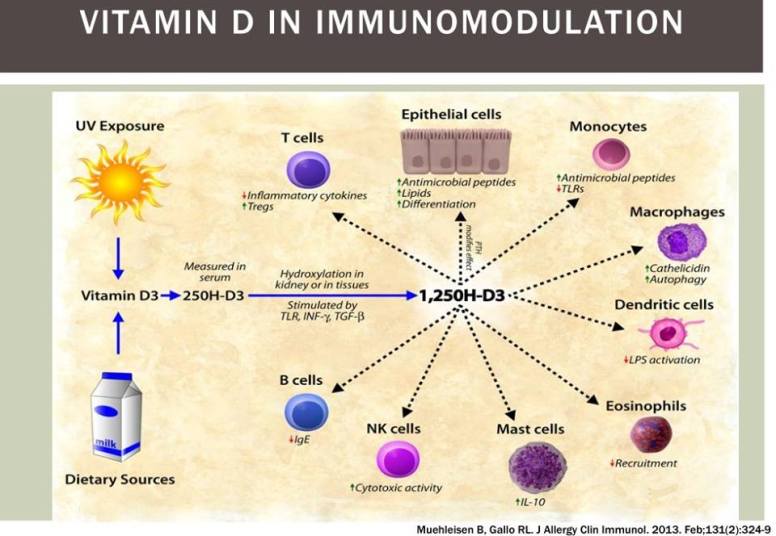
Also, Vitamin D alters the microbiome.
The classic study with CFS is by Hock, her’s [2009] update
What about toxicity? Well, it turns out that there have been very very very few cases of toxicity occurring — typically a prescription error had 50,000 IU/d and three months later, toxicity appear — which disappeared with stopping the vitamin D. A list of all of the known cases is here [2011], another case had 200,000 IU/d and toxicity appeared after two months.
“According to Dr. Heaney, there are no reported cases of elevated serum calcium below 30,000 IU’s of vitamin D per day, and for the most part, there are none below 50,000 IU’s.” [Dr. Mercola]
