This weekend I received this email from a reader (quoted in full — as received):
Hi Ken,
I was wondering if you would be willing to review my uBiome sample and provide me some feedback. Feel free to share my results on your website. To give you a little bit of background, I have been diagnosed with IBS and more recently CFS. My mothers side of the family has a lot of GI issues. Half (7/14) have been diagnosed with IBS or Crohns with some having very serious cases of Crohns.
Back in March I had to take time off work because my energy levels were so low that I could barely do anything. During that time I followed many of your suggestions on herbs and probiotics. I cycled through the following probiotics: Mutaflor (I could not take this for very long as it gave me bad stomach pain), Symbioflor 1 and 2, Prescript Assist, GB Equilibrium, L fermentum ME3, AOR-3 and Align. The only ones that produced any herx were PA and Symbioflor 2 and they produced fairly significant herx. I did have minor herx while I was taking Align, AOR-3 and GB together in large amounts but it didn’t last very long, only a couple days.. The herbs I tried were: Neem, Tulsi, Oil of Oregano, harataki, coconut oil, licorice, turmeric and olive leaf. I had some herx from Neem, Tulsi and licorice but it was very little and only lasted for a couple days for each. I increased the doses quite a bit but still got no added herx. When all of these probiotics and herbs no longer had any effect on me, I stopped taking them. Since then my energy levels have improved significantly where I am now able to work again. Thank you so much! I honestly can’t thank you enough because I really do feel like you have saved my life. I have been to the mayo clinic, nutritionists, naturopaths, I have done an all liquid Vivonex diet, FODMAPS, quit sugar, gluten, alcohol, dairy and carbs, etc. etc. My wife and I have easily spent over $25 000 to try to improve my condition in the past three years.
Prior to taking these probiotics I was extremely gluten sensitive. A few years ago, at the suggestion of a nutritionist I quit eating gluten. Only four days after quitting, I accidentally ate some gluten and I got extremely sick. Within 10 minutes, my stomach bloated out an extra 3 inches, I got a really bad headache, lightheaded and dizzy, really bad stomach ache, my skin got really dry, I got really depressed and I started to dry heave. This happened every subsequent time I accidentally had gluten. Last month I accidentally had gluten and nothing happened. I am now able to eat gluten. I think this really hits home to your post earlier in the week about how the person isn’t gluten sensitive but their microbiome is. Sorry if I’m going off on a tangent but I thought you might find this information interesting. I would not consider myself in remission because I still have bad days and even my good days I feel like I’m only about 75-80% but this is such an improvement that I feel like I have my life back. I was wondering if you would consider having a look at my results and offering any opinions on where I could improve my gut bacteria so I could potentially further improve my condition.
uBiome Result Review
Despite the probiotics, the classic two items are still low:

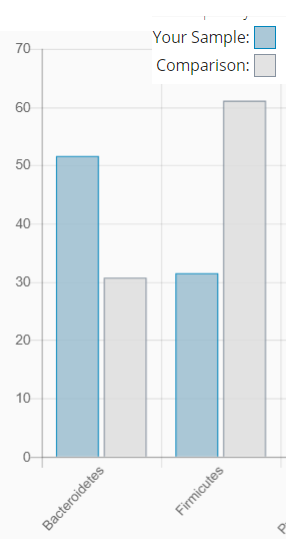
Akkermansia was 220% of typical results. The ratio of Bacteroidetes to Firmicutes is still far from normal.
As seems to be common, biodiversity is high (88%ile) – but less than many uBiomes that I have seen. In terms of most uncommon bacteria (i.e. < 5% of sample), his is lower than is usually seen, a good sign. Note all of these are less than 2% of the level found in those that have these bacteria.
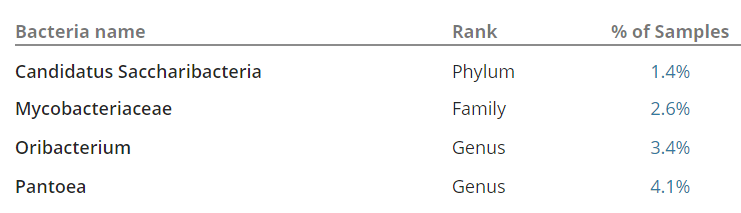
The Candidatus Saccharibacteria is very interesting because it has a parasitic phase (killing it host bacteria) and has been isolated from the human oral cavity.
- It “associated with human diseases such as periodontitis and inflammatory bowel disease (IBD) ” [2014]
- It may be reduce by Azithromycin [2016]
- Hint: if you want to go the antibiotic path, you may find dentists are more cooperative than many MDs… if it is for periodontitis issues [do not oversupply information].
- It is involved in many many KEGG pathways (see site)
Oribacterium is also found in the human oral cavity. [2014] “Susceptible to kanamycin, vancomycin, metronidazole, penicillin, rifampicin and bile but resistant to colistin.”
Concern: while there are low in the gut results, the usual origins of them are the oral cavity suggesting that there may be an overgrowth of there there.
Overgrowths

Erysipelotrichia appears to increase with high fat diet [2011] [2017], so reducing fat intake — reduce beef and pork, increase chicken, turkey and rabbit. Alphaproteobacteria is also associated with high fat diet [2015]. Betaproteobacteria is associated with diabetes risk [2012].

Again, all of high ones were associated with high fat intake.


Dielma (part of Clostridiaceae bacterium) is of special concern, unfortunately I could find nothing specific for diet. ” D. fastidiosa is susceptible to amoxicillin, imipenem, metronidazole and ciprofloxacin, but resistant to trimethoprim/sulfamethoxazole, rifampin, doxycycline and gentamicin.” [2013] Based on CFS patients reports listed here, I would seek a course of metronidazole, followed by a course of ciprofloxacin (a fluoroquinolones) from my MD (actually a ND in my case).
Bottom Line
This person has seen some dramatic changes. From becoming gluten sensitive to being able to consume gluten again. From being unable to work, to returning to work. His uBiome is reasonable for 70% recovery. It is not as good as the last uBiome review where the person felt that he had effectively recovered.
Using the model, he has successfully suppressed many of the bacteria that was causing symptoms. The very important word is suppressed – not eliminated. My view of the “bad bacteria” is that they should be thought of as a virus. You never eliminate the virus, rather your system learns to keep it in control.
I would advocate continued rotation of herbs and probiotics for at least 6 months. I still rotate them – I keep a cup of triphala or neem tea; I usually take one probiotic for a one week cycle. If I forget, I do not get uptight about it. However, whenever I get anything suggesting stomach upset or a cold or flu… then I load up quickly (which seems to have the additional benefit of shortening the duration).
Discussion with their MD on getting the two candidate antibiotics cited above is recommended. As always, always discuss any changes with your knowledgeable medical professional.
