The vast majority of papers were repeats of prior research (earlier research was in 1992 for some topics). The following were more interesting:
- Understanding, diagnosing, and treating Myalgic encephalomyelitis/chronic fatigue syndrome – State of the art: Report of the 2nd international meeting at the Charité Fatigue Center [2023]
- An Explainable Artificial Intelligence Model Proposed for the Prediction of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and the Identification of Distinctive Metabolites [2023]
- “The metabolomics of C-glycosyltryptophan, oleoylcholine, cortisone, and 3-hydroxydecanoate were determined to be crucial for ME/CFS diagnosis.”
- The items identified are associated with other conditions too (see links). Prediction is not treatment.
- DNA Methylation Changes in Blood Cells of Fibromyalgia and Chronic Fatigue Syndrome Patients [2023]
- “Methylomes of the blood cells of patients with FM and CFS in three independent studies have shown methylation changes that appear to be implicated in the pathogenesis of these syndromes.”
- Well known, see MEPedia, treatment based on this hypothesis has not been effective for most
- Myalgic encephalomyelitis/chronic fatigue syndrome and fibromyalgia are indistinguishable by their cerebrospinal fluid proteomes [2023]
- People with Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Exhibit Similarly Impaired Vascular Function [2023]
- ” both long COVID and ME/CFS patients exhibit similarly impaired endothelial function, indicating potential vascular involvement in the pathogenesis of these post-viral illnesses. The significant reduction in flow-mediated dilation values suggests an increased cardiovascular risk”
- Increased gut permeability and bacterial translocation are associated with fibromyalgia and myalgic encephalomyelitis/chronic fatigue syndrome: implications for disease-related biomarker discovery [2023]
- “Biomarkers of intestinal barrier function and inflammation were associated with autonomic dysfunction assessed by COMPASS-31 scores in FM and ME/CFS respectively. Anti-β-LGB antibodies, ZO-1, LPS, and sCD14 may be putative predictors of intestinal barrier dysfunction in these cohorts.”
- Well known from prior studies, causality not explored.
- Brain-regional characteristics and neuroinflammation in ME/CFS patients from neuroimaging: A systematic review and meta-analysis [2023]
- “Regional alterations were most frequently identified in the cerebral cortex, with a notable focus on the frontal cortex. However, our meta-analysis data revealed a significant hypoactivity in the insular and thalamic regions, contrary to observed frequencies. These abnormalities, occurring in pivotal network hubs bridging reason and emotion, disrupt connections with the limbic system, contributing to the hallmark symptoms of ME/CFS.”
- This is a repeat of prior research going back to 1992
- Many studies with “Some patients …” with specific abnormalities
- A Quick and Practical Approach to Secure a Chronic Fatigue Syndrome Diagnosis: The Novel Functional Limitation Index [2023]
- “The Functional Limitation Index (FLI) could provide an easy and accurate diagnosis of this condition in both genders in a one-day assessment.”
- Effects of traditional Chinese mind-body exercises for patients with chronic fatigue syndrome: A systematic review and meta-analysis[2023]
- “In patients with CFS, TCME probably reduces post-intervention fatigue, depression, and anxiety and may improve sleep quality and mental function compared with passive control, but has limited long-term effects. “
- Frontiers in chronic fatigue syndrome research: An analysis of the top 100 most influential articles in the field [2023]
- “The prospective research directions in this field include the search for biological markers, with a particular focus on immunology; the advancement of diagnostic techniques; the screening of risk genes associated with CFS; and the conduct of epidemiological investigations.”
- So treatment does not seem to be an active dimension.
- Onset Factors:
- Increased risk of chronic fatigue syndrome following infection: a 17-year population-based cohort study [2023]
- “infection with common pathogens, including bacteria, viruses, is associated with an increased risk of developing CFS.”
- This matches my model that ME/CFS is a post-infection persistent microbiome dysfunction.
- Genetic risk factors for severe and fatigue dominant long COVID and commonalities with ME/CFS identified by combinatorial analysis [2023]
- Genetics have long been identified as a factor
- Typing myalgic encephalomyelitis by infection at onset: A DecodeME study [2023]
- There is an overlap between long covid and ME/CFS.[2023]
- Increased risk of chronic fatigue syndrome following infection: a 17-year population-based cohort study [2023]
- Is there a role for traditional and complementary medicines in managing chronic fatigue? a systematic review of randomized controlled trials [2023]
- “recommendations of T&CMs in treating CFS remain inconclusive. To develop better quality evidence about T&CMs for CFS, future studies should employ more objective diagnosis standards and outcome measurements, larger sample size, and better bias control, and ensure the compliance with the corresponding reporting guidelines”
- I have seen this constantly in studies: too small sample size, poor statistical analysis, spinning results to “find something”.
- Treatment:
- Successful treatment of myalgic encephalomyelitis/chronic fatigue syndrome using hydrogen gas: four case reports [2023]
- “In conclusion, since this was a case study based on self-assessments by a small number of patients and not a clinical study”
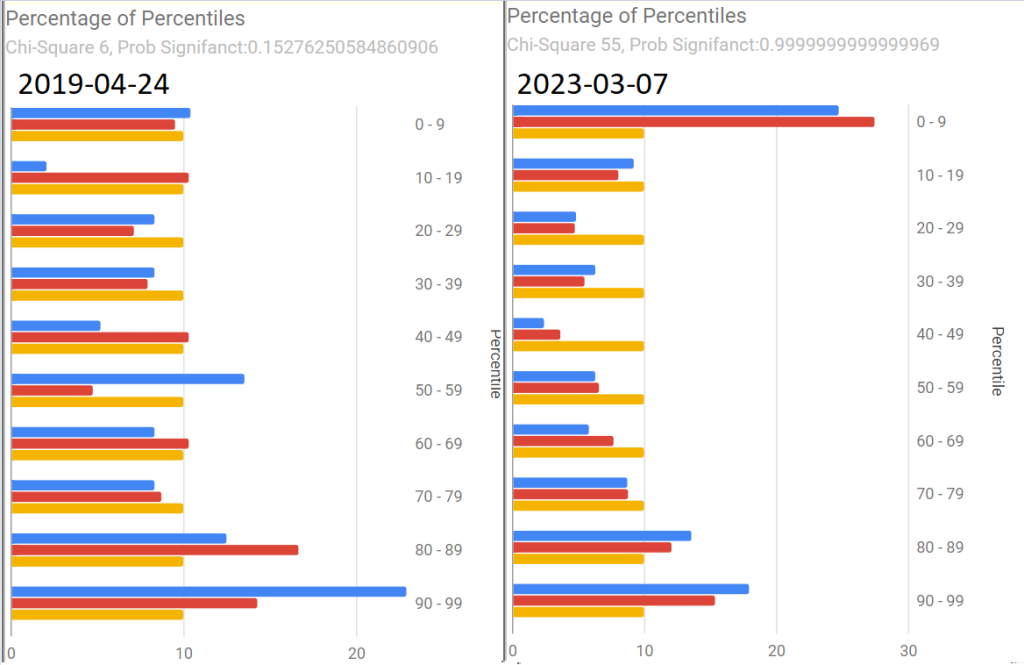
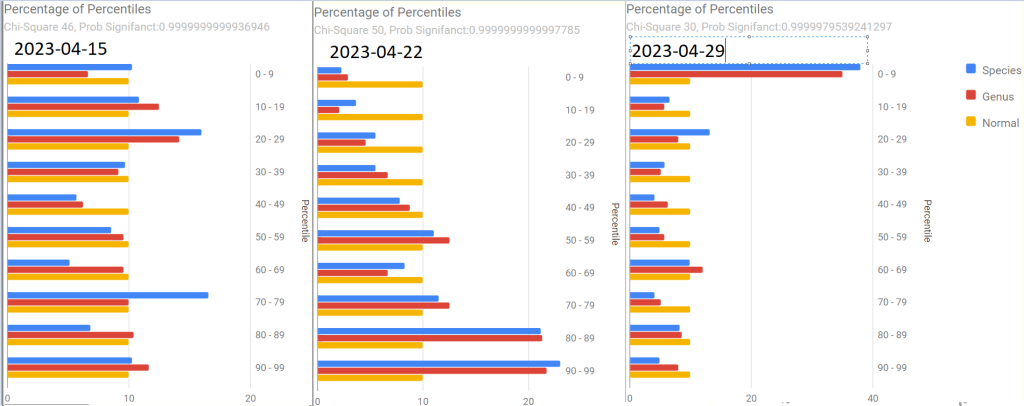
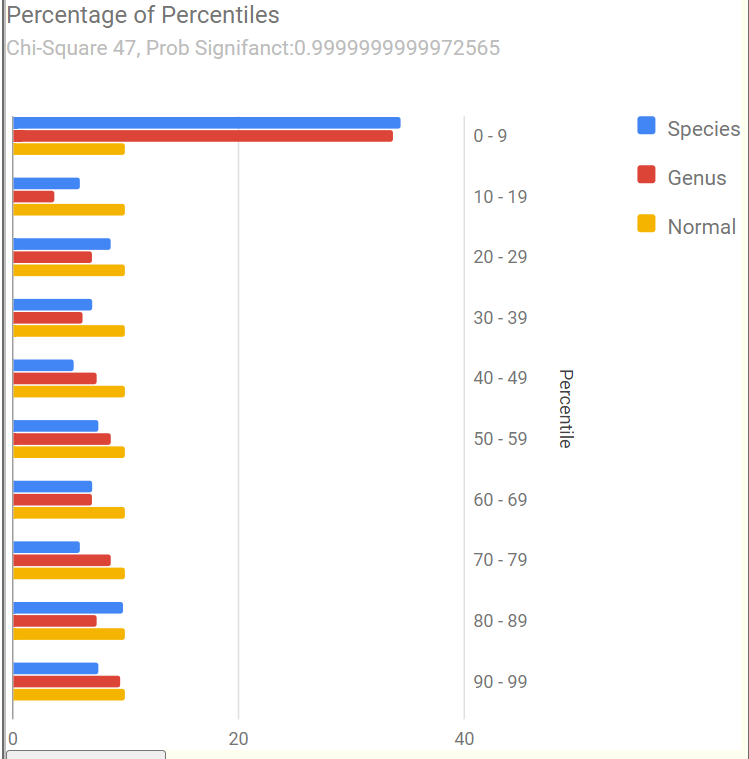
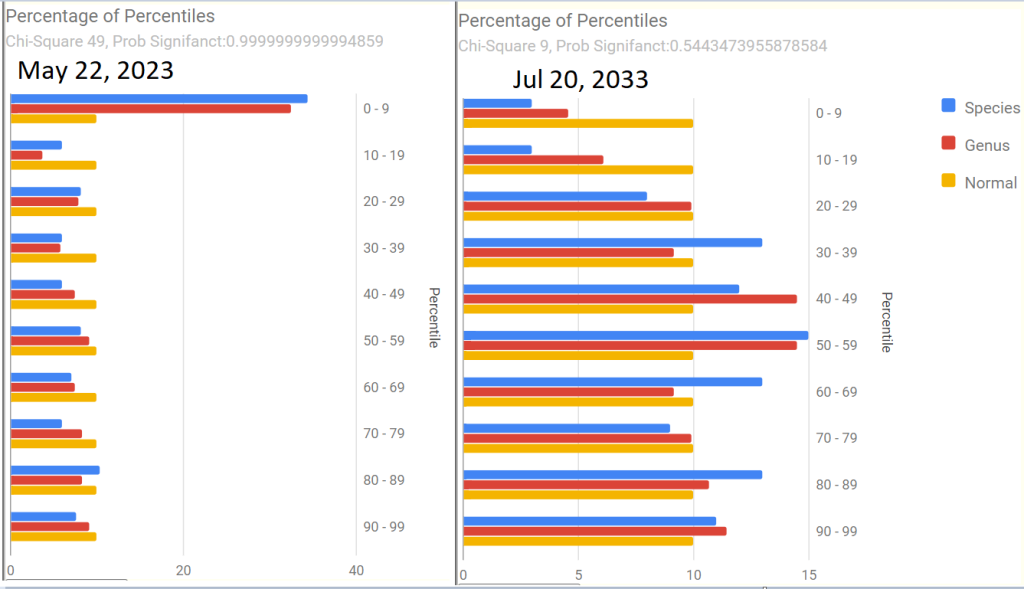
- Hydrogen is a gas used by bacteria (illustrated by SIBO testing for Hydrogen), this approach is likely to influence the microbiome. Looking at the data on Microbiome Prescription, we found that ME/CFS patients microbiome has a significantly higher consumption of Hydrogen — thus the extra hydrogen may alter the microbiome.
- B-vitamins, related vitamers, and metabolites in patients with quiescent inflammatory bowel disease and chronic fatigue treated with high dose oral thiamine [2023]
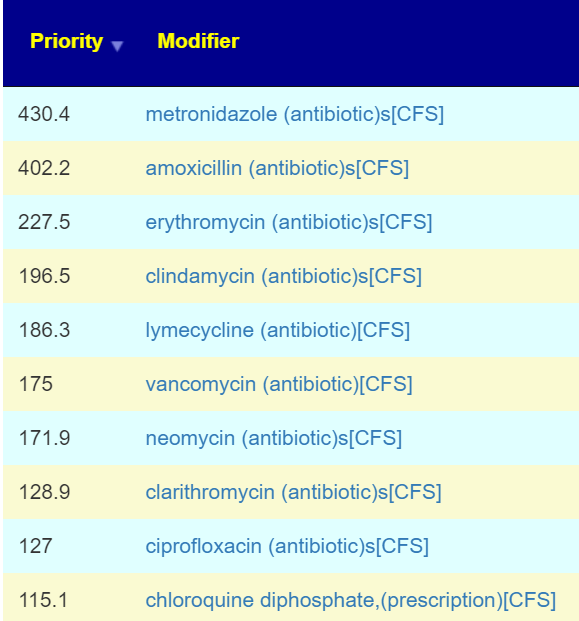
- Glucan (or foods containing it: Barley etc) is a very frequent suggestion from Microbiome Prescription when a ME/CFS microbiome was processed through microbiome prescription.
- Repetitive transcranial magnetic stimulation ameliorates symptoms in patients with myalgic encephalomyelitis (chronic fatigue syndrome) [2023]
- Some symptoms improved: “orthostatic intolerance with the inability to complete the 10-min standing test was resolved in 10 (83%) out of 12 patients, and disequilibrium was resolved in 15 (88%) out of 17 patients. “
- Yeast Beta-Glucan Supplementation with Multivitamins Attenuates Cognitive Impairments in Individuals with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial [2023]
- Beta-Glucan (or foods containing it: Barley etc) is a very frequent suggestion from Microbiome Prescription when a ME/CFS microbiome was processed through microbiome prescription.
- “significantly improved cognitive fatigue (assessed with FIS-40 scores) after the 36-week treatment
- Successful treatment of myalgic encephalomyelitis/chronic fatigue syndrome using hydrogen gas: four case reports [2023]