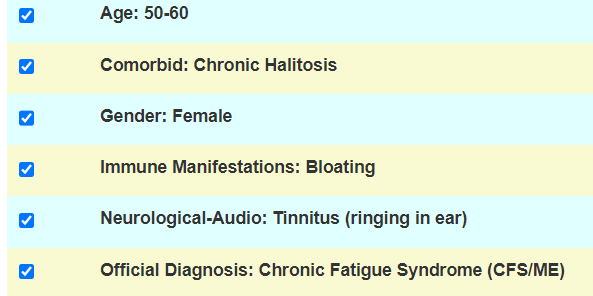
A reader wrote me today with the following question
I read your article on microbial involvement, can you explain in more detail why you recommended cutting out Lactobacillus? If I interpreted your analysis, you said lactobacillus was rare in ME/CFS, doesn’t that mean increasing it could be beneficial? “..lactobacillus shows up barely in only one result..”.Meaning lactobacillus is rare for ME/CFS patients?
I meant that there is no clear evidence of a lactobacillus deficiency with ME/CFS patients microbiomes. There are reasons to believe that it may be harmful and helps maintain ME/CFS state.
History
I am a facts/study based individual that have been reading studies, conference reports since 1990’s. Back in 1999, on eGroups CFSFM-Experimental, taking probiotics were often suggested. Why? Because probiotics has been promoted as a cure-all for all conditions. A influencer snake oil. Reported results on CFSFM-Experimental were disappointing.
My mind proceeded logically. So ask the US National Library of Medicine (PubMed), “Which probiotics have been helpful for ME/CFS? Given that there were 2400 studies on ME/CFS then, I expected to find a few dozen by then — after all, it would likely be one of the first choices by naturopaths who would rush to publish their results!! There were none that used lactobacillus probiotics. Even today, we have just 32 studies mentioning “chronic fatigue syndrome” probiotics in the 8500 studies posted. [Sarcasm] “Surely, there would have been a rush with all of the ME/CFS specialists to use lactobacillus probiotics given all of this evidence”.
Being a scientist, I know that what gets published are positive results — not no result nor negative results.
Reading conference papers presented by specialist on ME Research UK, I came across a report of a conference panel by active practitioners where the consensus was no benefit. I have worked as a professional technical writer and very “phrasing aware”, I read the wording to indicate that probiotics likely did harm in some of their patients. Slamming probiotics tend to be view as a heresy with many health influencers.
There Appears No Significant Objective Evidence that lactobacillus helps!
Yes, you will find testimonials — but that is not objective evidence. They may have helped because the person did not have ME/CFS (self diagnosis) or a different condition. It is incomprehensible that there have not been dozens (or hundreds) of studies trying lactobacillus — studies that are unpublished because of unfavorable results.
Why may it be EVIL?
Again, conference papers from Australia’s Alison Hunter Memorial Foundation play an important role here. From the Way-Back machine I retrieved items no longer on their site and pasted it into 1998 Was a very good year…. The key finding was “The mean distribution of E.coli as percentage of the total aerobic microbial flora for the control subjects and CFS patients was 92.3% and 49% ” Not a little drop, but almost half the level!
NOTA BENA: The typical (cheap) 16s tests used for most modern microbiome studies effectively ignore E.Coli. Shotgun testing (much more expensive) finds E.Coli in almost every sample. Some 16s finds it in 1 in a thousand samples as shown by the table below. Modern studies not repeating these results is a direct consequence of their methodologies!!
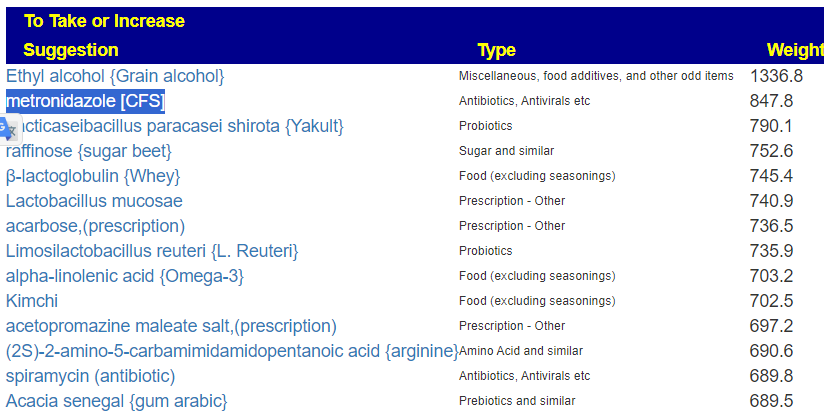
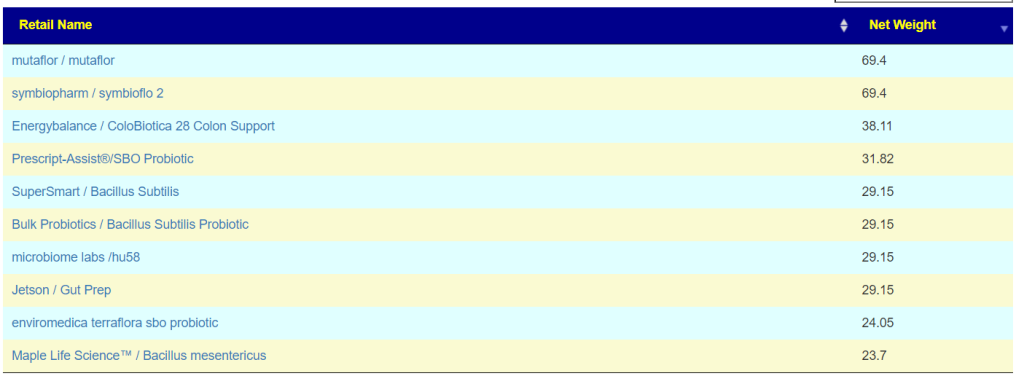
This was the motivation for my trying Mutaflor Probiotics (E.Coli Nissle 1917) which I happen to have in the house because my wife has Crohn’s and it made a huge difference for her (with lots of studies reporting it too!!!). I had a severe Jarisch–Herxheimer reaction for two weeks and a rapid recovery from ME/CFS afterwards.
If you look at Odds Ratios for Metabolites and ME/CFS, you will see that E.Coli probiotics has the biggest impact on the metabolite imbalance with ME/CFS

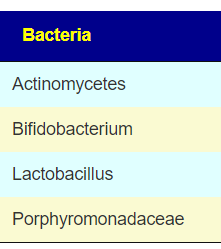
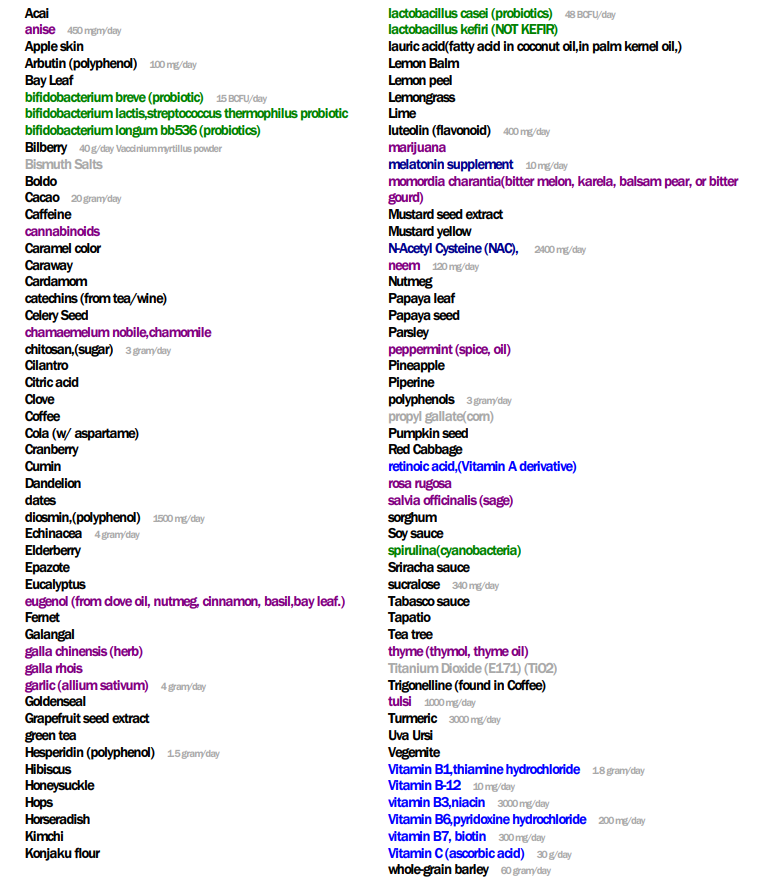
Going over to the E.Coli page on Microbiome Prescription we see that Lactobacillus constantly reduces E.Coli. So we are moving from levels that are 50% of normal levels to even lower levels.

IMHO, for ME/CFS, Lactobacillus probiotics are EVIL
Yes there are a few lactobacillus that will help some symptoms (and likely make other symptoms worse). Unless you are very sure that it has the actual probiotic strain used in studies, don’t do it. See Probiotics — what is advertised may not be what you get.
IMHO, for brain fog, Lactobacillus probiotics are EVIL
- Probiotic use is a link between brain fogginess, severe bloating [2018]
- Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis [2018]
- “Of particular concern is the association between certain probiotic strains, such as Lactobacillus species, and the production of bacterial metabolic byproducts (e.g., D-lactate and histamine) implicated in the pathogenesis of brain fogginess, a term describing a state of cognitive dysfunction characterized by symptoms including confusion, impaired judgment, and lack of focus ” [Aug 2024] with many links to further studies.
Interesting study relative to ME/CFS and brain fog. Lactobacillus can trigger “thick blood”, decreasing oxygen delivery (hypo perfusion). The aggregation of human platelets by Lactobacillus species
This extends to a few other Conditions
- Increased Proportions of Bifidobacterium and the Lactobacillus Group and Loss of Butyrate-Producing Bacteria in Inflammatory Bowel Disease [2014]
- Bifidobacterium and Lactobacillus Counts in the Gut Microbiota of Patients With Bipolar Disorder and Healthy Controls [2019] Which found that more Lactobacillus resulted in poorer sleep.
Bottom line, checking for clinical studies if a probiotics clearly helps is recommended. This search engine may help.
Bifidobacterium also?
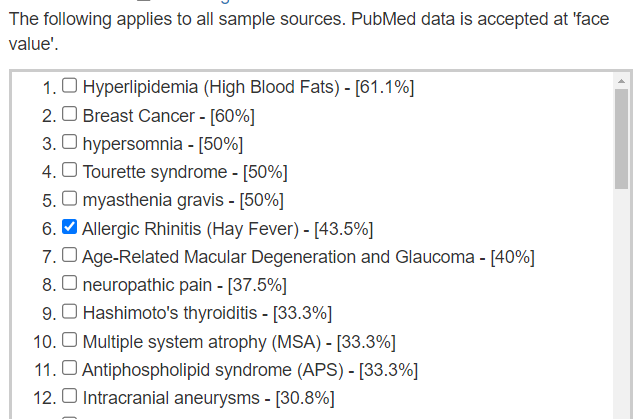
In Visual Exploration of Odds Ratios, we see that ME/CFS people have higher then general population amounts of Bifidobacterium. On the flip side, the average amount is reported lower on several studies. This compounds issues with several things that needs to be investigated.
- Did the lower bifidobacterium count not found in their average as zero? We use the values only when detected. Looking at the dots, we see that the dots are sparse/rare for lower values suggesting a lower detection rate. This suggests a threshold behavior of bifidobacterium.

Looking at impact on E.Coli, we see most studies say that it decreases E.Coli

There is not enough data to come to a safe conclusion.