In the family dealing with ME/CFS we were very fortunate in working with now retired folks, (links to MEPedia pages on them). It was 25 years ago.
- Byron Hyde MD, Canada
- David Bell MD. US – Created the Bell disability scale for ME/CFS
- David Berg — I hosted several online chats with him. He is now retired
Also we had significant interaction with
- Cecile Jadin MD, South Africa – by email. Still practicing
- Garth Nicolson Ph.D. US – I was on a TV News Program with him
Many support groups provide lists of local MDs that are sympathetic to ME/CFS patients. Typically, they will attempt to do symptom relief, not remediate the underlying cause or do not test outside of their local standards of practice (i.e. testing for associated viral infection, Lyme or rickettsia infections) – independent of insurance coverage or the patient being will to pay.
For example:
- For Washington State, Best Chronic Fatigue Syndrome Doctors in Seattle, WA. The heathgrade site covers most US states.
- Note: the grades tend to indicate friendliness, not effectiveness of treatment.
- Chronic fatigue – Internal medicine specialists – Edinburgh
The family was extremely fortunate to be covered by the old Microsoft Medical insurance that covered everything that the MD wanted with no deductibles; and we had a MD that was willing to learn and explore.
My recommendations for books are:
- Understanding Myalgic Encephalomyelitis, Byron Hyde MD
- The Clinical and Scientific Basis of Myalgic Encephalomyelitis – Edited by Byron Hyde, M.D.
Free Download eBook (PDF) This is a collection of a massive number of early research papers — most still relevant. - Other publications worth a review: https://www.nightingale.ca/publications
Other books can be found here:
- Goodreads: Me Cfs Books, I would exclude books not written by a MD or published before 2020.
Note that the better books are often difficult or impossible to understand due to brain fog (and sometime lack of sufficient education is specific areas)
Determine a Model and if possible, see if there is evidence that the model works
I went with two models for ME/CFS: A hypercoagulation condition (David Berg) and an “occult rickettsia like infection” (Cecile Jadin); today we could call it “post Infection Fatigue Syndrome”. Both were testable (by lab or by reaction to low risk drugs, i.e. an antibiotic often prescribed for Acne) and actionable.
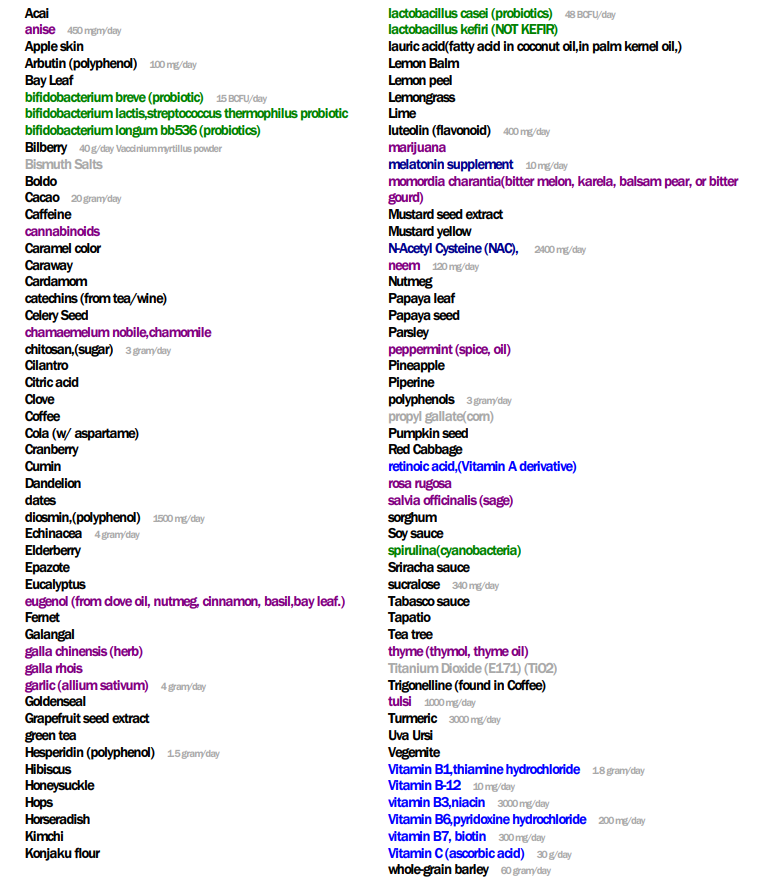
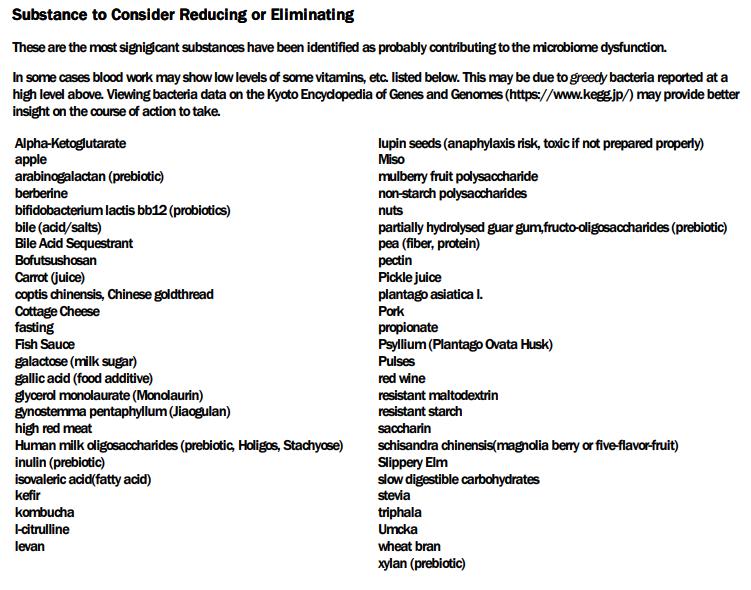
Today, my thinking is that the simplest model is a persistent microbiome dysfunction. This is very testable with direct retail tests; and actionable (using Microbiome Prescription). Often the antibiotics suggestions from Microbiome Prescription mirrors the Jadin approach. The treatment plan works for her models and my microbiome model!
Going with a hypothesis that is not both testable and actionable is not recommended. Take action today incase it works! Leave speculations to researchers trying to get grant money for their special interests.
For examples using my model: see Analysis Posts on Long COVID and ME/CFS
Symptoms and Bacteria appears to be strongly related
It is typical that Microbiome Prediction correctly predicts 80-100% of a person’s dominant symptoms from their microbiome. This implies that the bacteria shifts are causing the symptoms; thus correcting the bacteria shifts may reduce or eliminate symptoms.
Suggested Questionnaire for Evaluating a MD
What testing would you like to do?
- I would expect these at least:
- Lyme Disease
- Rickettsial infections
- EBV, HHV5 and other virus in CFS
- Coagulation Testing (including inherited coagulation defects)
Are you going to just provide symptom relief or are you going to search for the underlying cause to eliminate it?