One of the common misconception is that there is a “normal” microbiome that can be used as a reference. Below is a chart from “Metagenomic sequencing of fecal DNA“. Diet makes a major impact on the distribution and volume of the bacteria.
- “In a study of gut bacteria of children in Burkina Faso (in Africa), Prevotella made up 53% of the gut bacteria, but were absent in age-matched European children.”[2010]
The chart below is for healthy individuals in 12 different countries. In some cases neighboring very similar countries (Sweden [SE] and Denmark [DK]) have very different compositions.
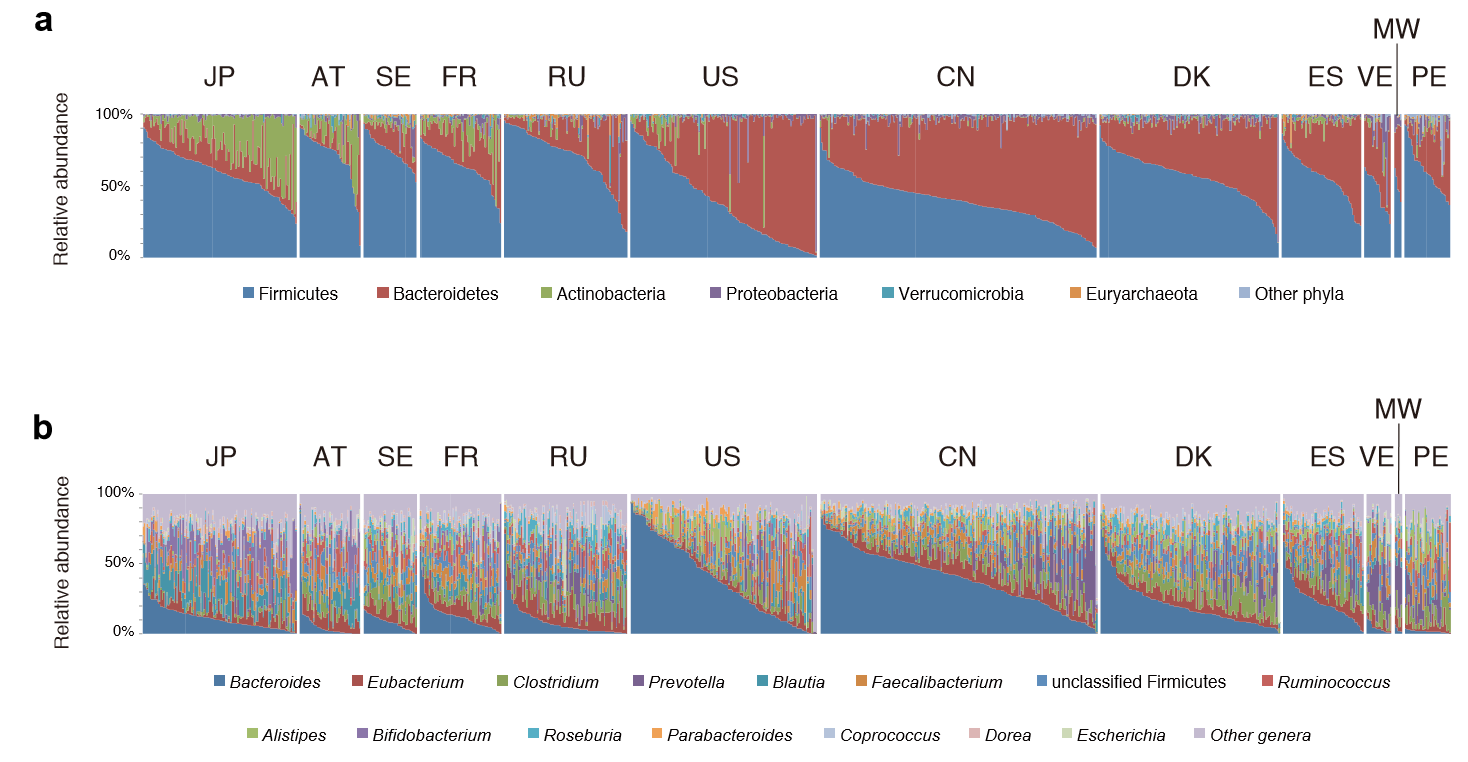
This great variation means that testing the microbiome can only be done as group of individuals living in the same area with similar eating habits…. An individual result without reference from people with the same eating habits and possibly ethnic background is very fuzzy to interpret. Yes, highlights may be common — like low E.Coli, Lactobacillus and Bifidobacteria…. but they likely apply to no more than 80-90%, the other CFS patients may have different shifts.
Then we also find that DNA also impacts the microbiome,
Host genetic variation drives phenotype variation, and this study solidifies the notion that our microbial phenotype is also influenced by our genetic state. We have shown that the host genetic effect varies across taxa and includes members of different phyla. The host alleles underlying the heritability of gut microbes, once identified, should allow us to understand the nature of our association with these health-associated bacteria, and eventually to exploit them to promote health.
Human genetics shape the gut microbiome , 2014
People have asked me, “Did you get your microbiome done, what was it?” My honest answer was “No, such testing was not available when I last had CFS. I simply assumed that my pattern would be an appropriate match to that reported from the 1998 Australian studies”
Age changes the microbiome
” DNA of the Clostridium leptum group and pathogenic Enterobactericeae increase in the gut microbiome with age and can be detected in the same individual’s coronary plaques along with pathogenic Streptococcus spp., associating with more severe coronary atherosclerosis. ” [2019]

The presence of the Bifidobacterium, Faecalibacterium, Bacteroides group, and Clostridium cluster XIVa decreased with age up to 66-80 years of age, with differences reaching statistical significance for the latter group. Interestingly, the levels of some of these microorganisms recovered in the very old age group (>80 years), with these older individuals presenting significantly higher counts of Akkermansia and Lactobacillus group than adults and the younger elderly
Age-Associated Changes in Gut Microbiota and Dietary Components Related with the Immune System in Adulthood and Old Age: A Cross-Sectional Study. [2019]
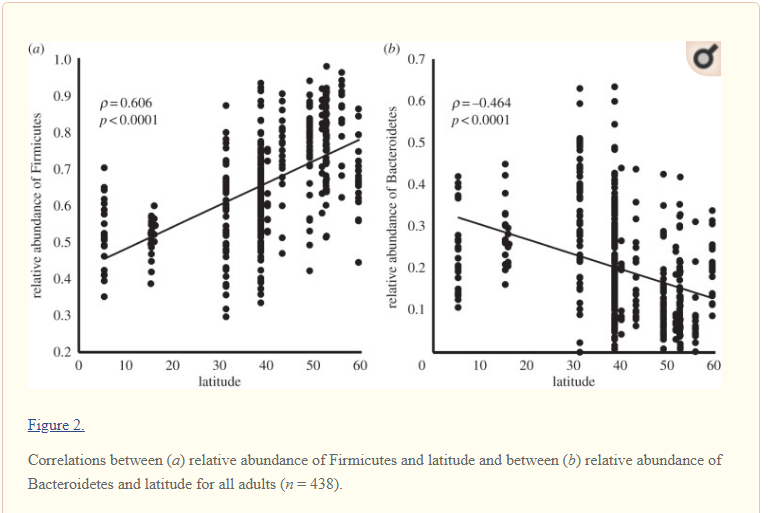
Latitude changes the Microbiome
Latitude means the distance from the equator. This may be due to sunlight-vitamin D levels.
If you exercised recently impacts the microbiome
Underlying these macro-level microbial alterations were demonstrable increases in select bacterial genera such as Veillonella (+14,229%) and Streptococcus (+438%) concomitant with reductions in Alloprevotella (-79%) and Subdolingranulum (-50%). To our knowledge, this case study shows the most rapid and pronounced shifts in human gut microbiome composition after acute exercise in the human literature.
Rapid gut microbiome changes in a world-class ultramarathon runner. 2019
Some Population Studies
“We analyzed the combined microbiome data from five previous studies with samples across five continents. We clearly demonstrate that there are no consistent bacterial taxa associated with either Bacteroides– or Prevotella-dominated communities across the studies. By increasing the number and diversity of samples, we found gradients of both Bacteroides and Prevotella and a lack of the distinct clusters in the principal coordinate plots originally proposed in the “enterotypes” hypothesis. The apparent segregation of the samples seen in many ordination plots is due to the differences in the samples’ Prevotella and Bacteroides abundances and does not represent consistent microbial communities within the “enterotypes” and is not associated with other taxa across studies.” [2016]
” All Egyptian gut microbial communities belonged to the Prevotella enterotype, whereas all but one of the U.S. samples were of the Bacteroides enterotype.
- The intestinal environment of Egyptians was characterized by higher levels of short-chain fatty acids, a higher prevalence of microbial polysaccharide degradation-encoding genes, and a higher proportion of several polysaccharide-degrading genera.
- Egyptian gut microbiota also appeared to be under heavier bacteriophage pressure.
- In contrast, the gut environment of U.S. children was rich in amino acids and lipid metabolism-associated compounds; contained more microbial genes encoding protein degradation, vitamin biosynthesis, and iron acquisition pathways; and was enriched in several protein- and starch-degrading genera.
- Levels of 1-methylhistamine, a biomarker of allergic response, were elevated in U.S. guts, as were the abundances of members of Faecalibacterium and Akkermansia, two genera with recognized anti-inflammatory effects.
- The revealed corroborating differences in fecal microbiota structure and functions and metabolite profiles between Egyptian and U.S. teenagers are consistent with the nutrient variation between Mediterranean and Western diets.” [2017]
“This suggests that similarities between the Inuit diet and the Western diet (low fiber, high fat) may lead to a convergence of community structures and diversity. However, certain species and strains of microbes have significantly different levels of abundance and diversity in the Inuit, possibly driven by differences in diet.” [2017]
Bottom Line
IMHO: There is no clear definitive benefit from doing an individual microbiome testing — there is no reference that is reliable for it on an individual basis at a fine level of details. On the other hand, having results showing abnormalities help in several ways:
- It encourages you to make changes in eating which will usually be for the better
- It confirms that you have significant shifts and supports the concept that the gut is causing your symptoms.
” This work supports that sex is a critical factor in colonic bacterial composition of an aged, genetically-heterogenous population. Moreover, this study establishes that the effectiveness of dietary interventions for health maintenance and disease prevention via direct or indirect manipulation of the gut microbiota is likely dependent on an individual’s sex, age, and genetic background. ” [2019]
